Bird flu: pink eye and a cold for 4 more people. More cows infected. No one has a plan, unless the plan is to keep the story simmering till we need another pandemic
Why not ignore it? The cows recover after a couple of weeks and the people barely notice the illness. Would the chickens recover if we left them alone?
Bird flu snapshot: As the number of infected dairy herds mount, so too does pessimism about driving H5N1 out of cows
https://www.statnews.com/2024/07/15/bird-flu-snapshot-h5n1-infected-herds/
By Helen Branswell July 15, 2024
Bird flu snapshot: This is the latest installment in a series of regular updates on the H5N1 flu outbreak in dairy cows that STAT is publishing on Monday mornings. To read future updates, you can also subscribe to STAT’s Morning Rounds newsletter.
There are more human cases of H5N1 bird flu infection, and another state has joined the list of those with infected dairy cow herds.
Colorado announced over the weekend that five workers involved in the culling of chickens at an H5N1-infected poultry operation had tested positive for the virus. Four of the cases have been confirmed by the Centers for Disease Control and Prevention; the fifth is currently deemed “presumptive” positive because the individual’s test sample hasn’t yet reached the CDC. All five had mild symptoms — conjunctivitis and minor respiratory complaints. None required hospitalization.
Additional testing by the CDC is needed to fully characterize the viruses responsible for these infections. But assuming they are the same as the one circulating in cows (which has occasionally spilled over into poultry operations), these cases will bring to nine the number of human infections recorded since this outbreak was first detected in late March. The CDC, at the request of the state, is helping investigate the new human cases in Colorado.
And on Friday came news that another state had discovered a bird flu-infected herd. Oklahoma announced that a sample collected in April that was only recently tested was found to be positive. On Monday, the U.S. Department of Agriculture confirmed two positive herds from the state — which may in fact be an error.
Lee Benson, public affairs officer for the Oklahoma Department of Agriculture, Food and Forestry, said that one dairy operation in the state suspected it had H5N1 in its cows in April and took swabs from two barns on the property. It did not submit them for testing at the time. With the recent unfurling of a USDA compensation program for lost milk production on farms where cows have tested positive for bird flu, the dairy sent both swabs in to be tested, Benson said.
“I can tell you that the confirmed positive sample is from one Oklahoma dairy. There are two separate barns that milk the dairy cows, and one sample was collected from each barn,” he said.
STAT asked the USDA whether it would alter the number of positive herds from Oklahoma, but has not yet heard back.
Oklahoma called itself the 13th state to find H5N1 in dairy cattle, but in reality its place on the list should be lower. The specimens were collected on April 19, Benson said. At that point only eight other states had reported positive herds.
These new human and animal developments support a blunt risk assessment from the Norwegian Institute of Public Health, which gave voice to a rising sense of pessimism about the prospects for containing the H5N1 outbreak in cows in a recent report.
“There are no clear signs that the outbreak is or is about to come under control,” the 26-page document on the public health risks associated with the ongoing spread states plainly.
“The risk that the situation will not soon be brought under control is great,” it continues, adding that “the probability of … and persistent chains of infection is considered high.”
As for the consequences of continued spread, the report suggests that while the risk the virus currently poses to people is not great, it could rise if transmission in cattle persists.
“There is a low, but increasing probability of viruses developing the ability to infect effectively to and between people,” it says. “The probability increases with prevalence in animals and with the duration of ongoing animal-to-animal infection.”
The risk assessment, dated June 24, is rapidly converted into English by Google Translate for non-Norwegian readers.
It’s reflective of what appears to be a growing view, certainly abroad but likely in the U.S. as well, that H5N1 isn’t in any hurry to give up on its new hosts and nothing farmers or government agencies are doing seems to be hastening its departure. (There is also a fair degree of skepticism about how hard farmers or the agency leading the response, the U.S. Department of Agriculture, are working towards that end.)
Michigan, which has been the exemplar state in terms of its efforts to find and report affected herds and to gain the trust of wary farmers, had gone almost a month without reporting a new infected herd. On July 5, it announced a herd in Gratiot County, which has been battling both poultry and dairy cattle outbreaks since early May. Texas has gone three weeks without adding to its list of affected herds. That changed on July 8.
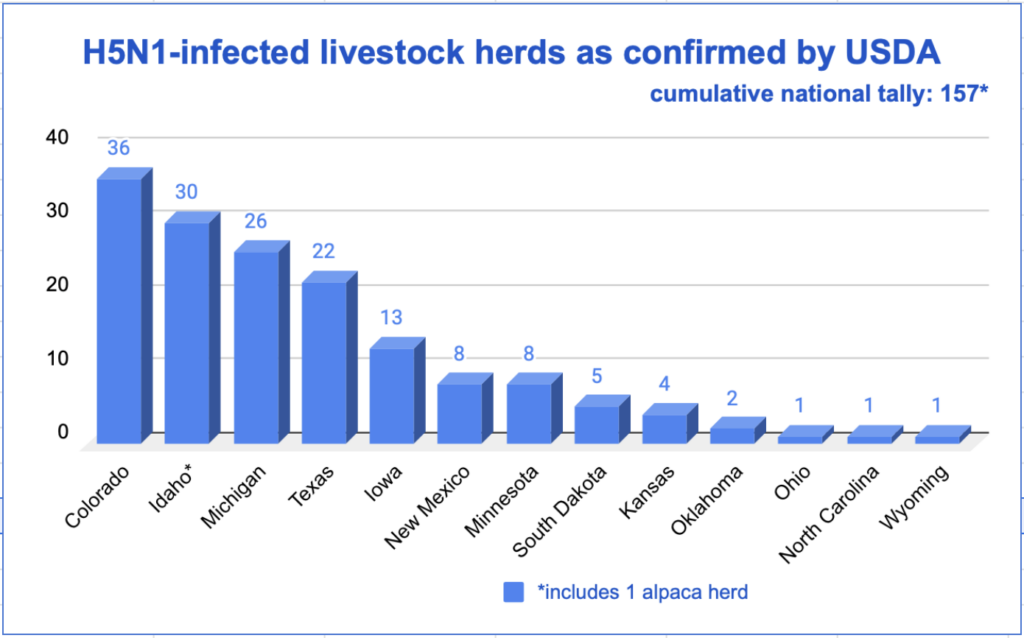
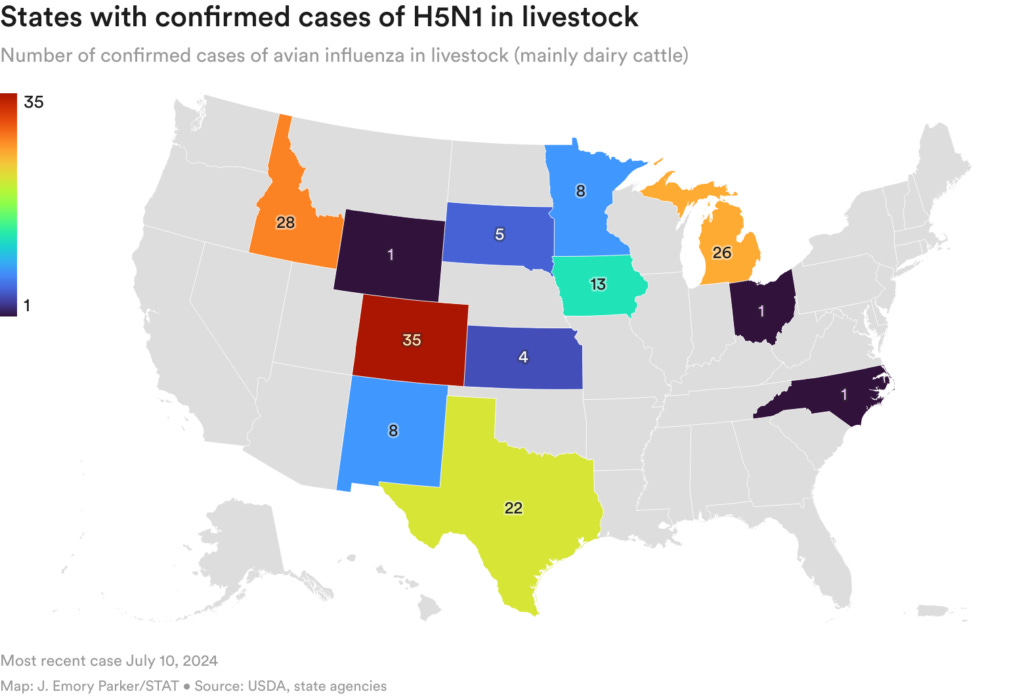
As of Monday, the USDA had listed 157 herds in 13 states as having tested positive for H5N1 since the outbreak was first confirmed in late March.
While the count of affected herds has risen steadily in a few of the reporting states — think Michigan, Colorado, Idaho — the number of states with dairy industries that haven’t reported a single outbreak puzzles experts monitoring this situation. (Some are downright dubious.) California, Wisconsin, New York, Pennsylvania, and Washington are on the top 10 list of dairy-producing states by revenue. Not one of those five has reported an affected herd.
Are they luckier? More vigilant? Do cows move around less frequently in those states? We don’t yet have those answers. But a news report from Missouri last week may help explain a possible difference between reporting and non-reporting states. (Missouri is one of the latter.)
Reporter Mary McCue Bell in the Columbia Missourian quoted a veterinarian with the Missouri Department of Agriculture’s animal health division saying that to date only 17 dairy cows — in a state that boasts 60,000 — have been tested for H5N1.
There’s a maxim in epidemiology: Seek and ye shall find. It would seem some states are not seeking.
The lack of a clear picture of how widespread the outbreak is in cattle continues to hamper efforts to assess whether this outbreak can be stopped and how best to do it if that end is within reach.
Asked Thursday if they thought the virus can be driven out of dairy cattle at this point, senior World Health Organization outbreak response leaders hedged their bets. Maria Van Kerkhove, acting director of WHO’s division of epidemic and pandemic preparedness and prevention, said at this point too little is known about the outbreak to make a prediction one way or the other.
“I think that’s a complicated question,” Van Kerkhove said during a WHO press briefing. “It doesn’t mean that it couldn’t happen. But I think that before we can get to an answer of when or if that could be possible, we need to understand the extent [of spread].”
And Mike Ryan, who heads the global health agency’s health emergencies program, said the ongoing presence of the virus in wild birds will continue to complicate efforts to control H5N1’s spread in domestic animals. It’s not just a question of driving it out, the goal needs to be keeping it out of an animal population — whether that’s poultry or dairy cattle. And that takes resources, surveillance, and long-term commitment from the veterinary, wildlife, and public health sectors, he said.
“And unfortunately in the world where we look for silver bullets and the treatment that will cure everything, unfortunately the treatment for most of our ills as a human civilization is cooperation, policy, resources and the will to do the job,” Ryan said.
Since USDA confirmed the presence of the virus in dairy cattle on March 25 there have been four confirmed and three presumptive human infections, all among farmworkers. All the individuals had mild symptoms; some had only conjunctivitis, while a few have had respiratory symptoms that resemble what is seen with infection with human flu viruses.
The announcement of the fourth case, on the eve of the July 4 holiday, led Adam Kucharski, the co-director of the Centre for Epidemic Preparedness & Response, at the London School of Hygiene and Tropical Medicine, to ask on the social platform X: “What’s the plan?”
Kucharski posed a bunch of hypotheticals — What if there are clusters of cases? Cases among people who haven’t had contact with cows? Cases exported to other countries? — to convey the point that a mere four years after the start of the worst pandemic since the 1918 Spanish Flu, the world does not appear to be grappling with the fact that H5 virus spreading in cows could lead to H5 virus spreading in people.
“What, here in 2024, is the plan for dealing with an outbreak of a potentially pandemic pathogen like H5N1?” he asked.
This article has been updated with new information from Oklahoma.





Other medical experts I follow say leave the birds alone and they'll end up with "natural immunity". You can NOT vaccine yourself or animals out of a respiratory virus infection. That's NOT how they work.
The Amish people don't do vaccines and instead rely on herd immunity and it works for them EVERY time.
Cooking meat from chickens and cows that may have been infected kills any viral infection they may have had.
OHMYGODNOOOOOOOO! Pinkeye! We’re all going to DIE of the pinkEYE! Are they serious? This one smells even worse than the ‘vid did. Anyone falling for this obvious cow patty has not been paying very close attention to what these evil mumphers have been doing these last almost 5 years.